Antibiotic resistance is a critical public health challenge where bacteria evolve to resist the effects of antibiotics, rendering once-treatable infections difficult or impossible to cure. The misuse and overuse of antibiotics in humans, animals, and farming have accelerated this problem, leading to longer hospital stays, increased medical costs, and higher mortality rates. If unchecked, common infections and minor injuries could once again become fatal.

What Is Antibiotic Resistance?
Antibiotic resistance occurs when bacteria evolve mechanisms to withstand the drugs designed to kill them or inhibit their growth. As bacteria become resistant, it becomes harder to treat infections, raising the risk of disease spread, severe illness, and death.
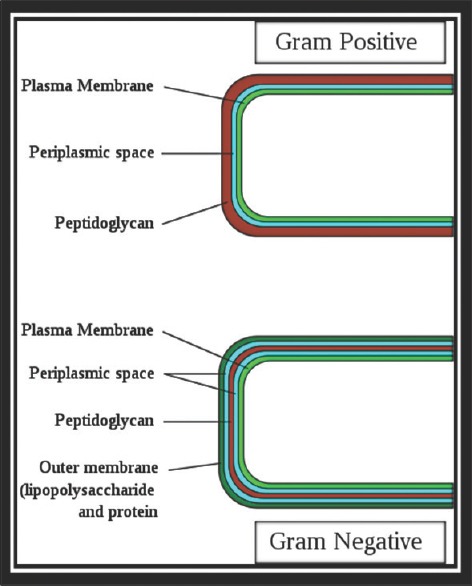
Structure of bacterial cell envelope
How Antibiotics Function
Antibiotics fight bacterial infections through several mechanisms:
- Damaging the Bacterial Cell Wall: Antibiotics like penicillin break down the bacterial cell wall, causing the bacteria to burst.
- Stopping Bacterial Reproduction: Other antibiotics, such as tetracyclines, prevent bacteria from multiplying.
- Disrupting Protein Production: Some antibiotics inhibit the production of proteins necessary for bacterial growth and survival.
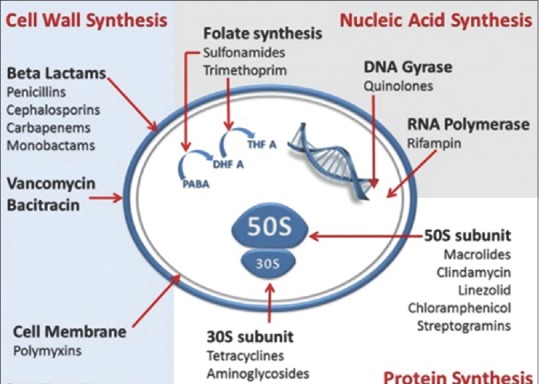
Mechanism of action of antibiotics
How Resistance Develops
Resistance arises through various processes:
- Mutations in Bacterial DNA: Random changes in bacterial DNA can lead to resistance by altering the drug’s target.
- Transfer of Resistance Genes: Bacteria can acquire resistance genes from other bacteria through processes like conjugation.
- Efflux Pumps: Some bacteria develop mechanisms to pump out the antibiotic before it can take effect.
- Enzyme Production: Certain bacteria produce enzymes that deactivate antibiotics, making them ineffective.
The Current Situation in India
Antibiotic resistance is particularly severe in India, with diseases like urinary tract infections (UTIs), pneumonia, and typhoid becoming increasingly difficult to treat. According to the Indian Council of Medical Research (ICMR), resistance is rising against commonly used antibiotics such as cefotaxime, ceftazidime, ciprofloxacin, and levofloxacin, particularly in bacteria like E. coli and Klebsiella pneumoniae.
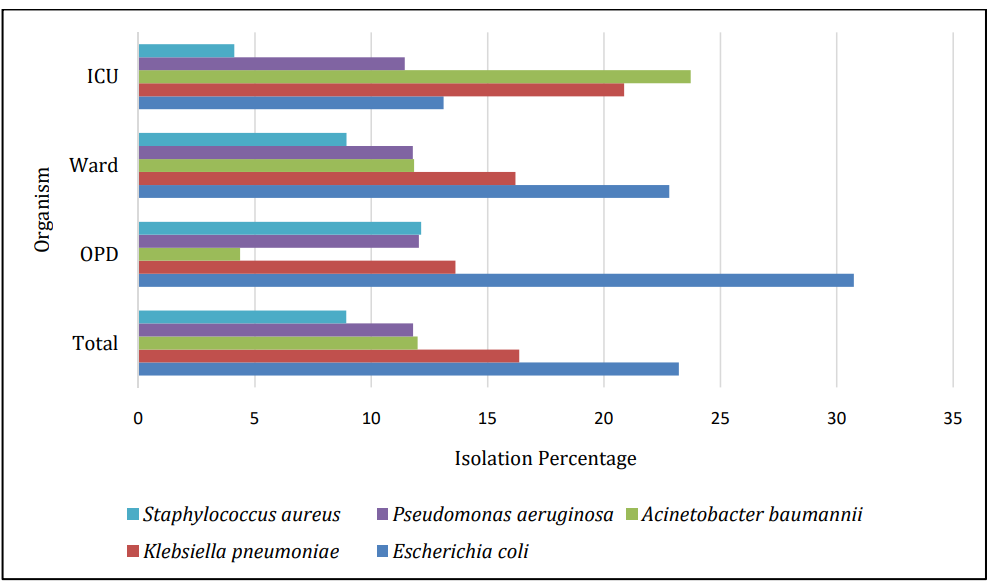
Distribution of top 5 isolates from all specimens across OPD, ward and ICU
Global Response and Recent Developments
Globally, several initiatives aim to address antibiotic resistance:
- UN and WHO Initiatives: The UN and WHO have prioritised antimicrobial resistance (AMR) at high-level meetings, calling for stronger international collaboration and the development of new treatments.
- Fungal Infections and the "Silent Pandemic": An increasing concern is resistance in fungal infections, with some experts dubbing it a "silent pandemic" that compounds the challenges posed by bacterial resistance.
Alternative Approaches to Fight Antibiotic Resistance
In response to growing antibiotic resistance, researchers are exploring innovative therapies:
- Phage Therapy: Phages, viruses that specifically infect bacteria, are being studied as a treatment for antibiotic-resistant infections.
- Probiotics: Introducing beneficial bacteria that can outcompete harmful, resistant strains is another avenue of research.
- Antimicrobial Peptides (AMPs): AMPs are short proteins that can destroy bacteria by disrupting their membranes.
- CRISPR-Cas: The gene-editing technology CRISPR-Cas is being tested for its ability to target and remove resistance genes in bacteria.
- Combination Treatments: Combining different antibiotics or therapies is another approach to counter resistance, often improving treatment outcomes.
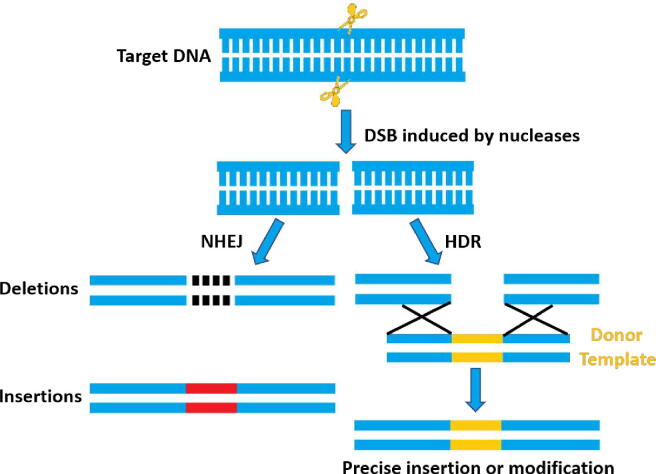
Mechanism of genome editing
Changes in Medications Due to Resistance
To stay effective, many antibiotics have evolved:
- Penicillin and New Variants: Penicillin was highly effective when first introduced, but resistance led to the development of newer versions such as amoxicillin and methicillin.
- Cephalosporins Generations: Cephalosporins, like cefotaxime and ceftazidime, have undergone several generations of development to combat resistant bacteria.
- Fluoroquinolones Development: Drugs such as ciprofloxacin and levofloxacin have been created to address resistance, particularly in respiratory and urinary tract infections.
Preventing Antibiotic Resistance
Preventing antibiotic resistance requires responsible use of antibiotics:
- Responsible Use of Antibiotics: Only take antibiotics when prescribed, complete the full course, and never use leftover antibiotics for new infections.
- Hygiene and Infection Prevention: Good hygiene practices, like frequent handwashing, help prevent the spread of resistant bacteria.

The Cost of Antibiotic Resistance
Antibiotic resistance poses a significant economic burden due to longer hospital stays, more complex treatments, and rising healthcare costs.
Case Studies
- Case Study 1: Drug-Resistant Tuberculosis in India: India has one of the highest burdens of drug-resistant tuberculosis (TB) globally, with an estimated 99,000 new cases of multidrug-resistant TB (MDR-TB) each year (WHO, 2011). Resistance rates are particularly high in reinfection cases, with some states showing a prevalence of 12-17%. Despite efforts by India's Revised National TB Control Program (RNTCP) to improve diagnosis and treatment, challenges remain due to limited lab capacity, inadequate treatment management, and drug shortages.
- Case Study 2: Methicillin-Resistant Staphylococcus Aureus (MRSA) in Hospitals: MRSA is endemic in India and poses a serious threat, especially in hospital settings. Studies show that MRSA is responsible for over 40% of Staphylococcus aureus infections in Indian hospitals, primarily affecting patients with skin, soft tissue, and bloodstream infections. Efforts to reduce MRSA transmission include improving infection control and promoting antimicrobial stewardship to prevent the spread of resistant strains. Source
The Role of Agriculture in Antibiotic Resistance
The agricultural sector plays a significant role in the spread of antibiotic resistance:
- Use of Antibiotics in Livestock: Antibiotics are frequently used in livestock to promote growth and prevent disease, contributing to the development of resistant bacteria.
- Environmental Spread: Antibiotic-resistant bacteria can spread through water, soil, and the food chain, posing risks to human health.
Global Cooperation and Policy Solutions
International cooperation is crucial in combating antibiotic resistance:
- International Regulations: Global policies aim to limit the overuse of antibiotics in both healthcare and agriculture.
- Research and Development of New Drugs: Pharmaceutical companies are encouraged to develop new antibiotics to stay ahead of bacterial resistance.
Conclusion
Antibiotic resistance is a growing global health crisis requiring urgent and sustained action. Both individual responsibility and international collaboration are essential to ensure that antibiotics remain effective. By understanding the causes and impacts of antibiotic resistance and adopting preventive measures, we can safeguard these critical medicines for future generations.
With inputs from agencies
Image Source: Multiple agencies
© Copyright 2024. All Rights Reserved Powered by Vygr Media.